What Makes Veins More Noticeable Under the Skin!
The human circulatory system is a marvel of biological engineering, a vast and intricate network of vessels that tirelessly transports life-sustaining blood to every corner of the body. Among these vessels, veins play the critical role of returning deoxygenated blood back to the heart. For many individuals, these pathways are not just internal concepts but visible realities, appearing as delicate blue, green, or purple lines tracing patterns beneath the surface of the skin. While the sudden prominence of veins can sometimes spark concern or self-consciousness, it is essential to understand that visible veins are, in the vast majority of cases, a perfectly normal and healthy manifestation of human physiology. The visibility of one’s vasculature is determined by a complex interplay of genetics, lifestyle, environmental factors, and the natural progression of time.
One of the most immediate and common reasons veins become more apparent is the body’s response to its environment and physical demands. When we engage in strenuous exercise, our muscles require a surge of oxygen and nutrients, leading to increased blood flow. This surge causes the veins to dilate—a process known as vasodilation—to accommodate the higher volume of blood returning to the heart. Similarly, external temperature plays a significant role. In warm weather or during a hot bath, the body seeks to cool itself by sending more blood toward the skin’s surface to dissipate heat. This thermal regulation makes the veins expand and appear closer to the surface. For athletes or individuals with low body fat, this visibility is even more pronounced, as there is less subcutaneous adipose tissue to cushion and obscure the vessels. In these contexts, visible veins are often a sign of a robust and active circulatory system working exactly as it should.
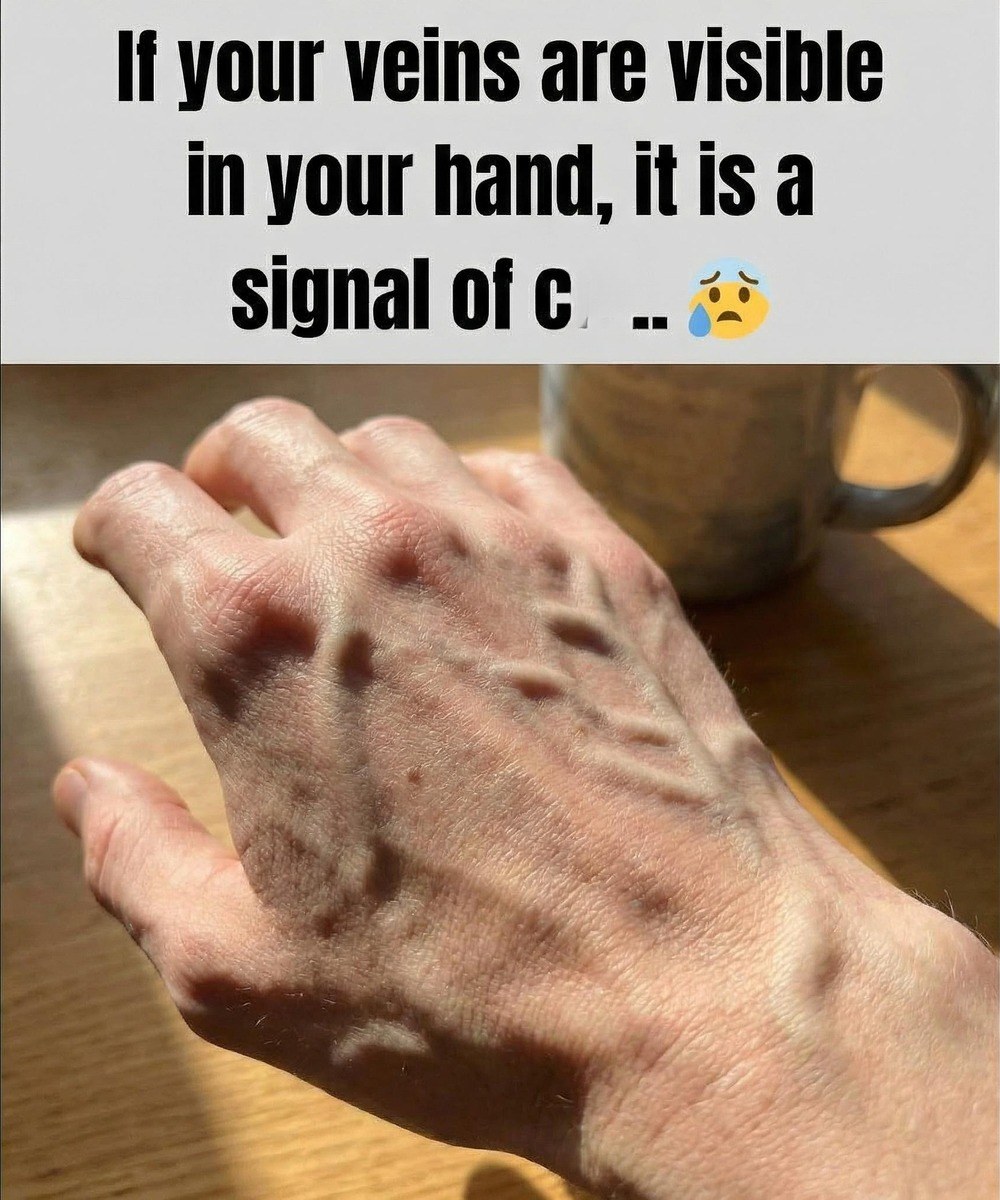
Beyond temporary environmental triggers, the natural aging process is perhaps the most universal factor in changing vein visibility. As we move through the decades, our skin undergoes structural transformations; it gradually loses collagen and elastin, the proteins responsible for thickness and resilience. As the dermis becomes thinner and more translucent, the underlying anatomy becomes more apparent to the naked eye. This is a standard biological shift and is typically most noticeable on the backs of the hands, the forearms, and the feet. Furthermore, genetics play a foundational role. Some individuals are simply born with fairer or thinner skin types that offer less “coverage” for their veins, a trait that is often inherited and entirely benign.
While most visible veins are simply a matter of aesthetics or temporary physiological shifts, there are times when their appearance reflects the internal mechanics of venous health. Within our veins are tiny, one-way valves designed to prevent blood from flowing backward as it fights gravity to return to the heart. When these valves become weakened or damaged—a condition often influenced by prolonged standing, sitting, or pregnancy—blood can begin to pool in the vessels. This accumulation of pressure causes the veins to become distended, twisted, or raised, leading to the development of varicose veins. Unlike the smooth, flat veins associated with exercise or thin skin, varicose veins often have a bulging, rope-like appearance and may be accompanied by a sensation of heaviness, aching, or throbbing in the lower extremities.
The development of more prominent or uncomfortable veins is often a cumulative result of various lifestyle factors. Modern life frequently requires us to remain in static positions for hours on end, whether sitting at a desk or standing on a retail floor. This lack of movement deprives the “calf muscle pump”—the rhythmic contraction of leg muscles that helps push blood upward—of its primary job. Over time, this chronic pressure can strain the vascular walls. Other factors, such as smoking, which damages blood vessel integrity, or carrying excess body weight, which places a heavier burden on the circulatory system, can exacerbate these changes. Hormonal fluctuations, particularly those associated with pregnancy or menopause, can also relax vein walls, making them more prone to stretching and visibility.